Professor Nick Anstey
Senior principal research fellow
Qualifications:
PhD, University of Western Australia, 2001; Fellowship of the Royal Australasian College of Physicians, 1992; Master of Science, University of London, 1989; Diploma of Tropical Medicine and Hygiene, London, 1989; Bachelor of Medicine and Bachelor of Surgery (Hons), University of Western Australia, 1985.
Approved level of HDR supervision at Charles Darwin University:
Principal Supervisor for PhD
Location:
Darwin - Royal Darwin Hospital campus
Biography:
Professor Nicholas Anstey is an infectious diseases physician at the Menzies School of Health Research in Darwin.
He collaborates with clinical and epidemiological research programs in Indonesia and Malaysia, and with malaria networks in the Asia-Pacific and Africa.
The goal of his translational research program is the reduction in morbidity and mortality from malaria. His research spans the epidemiology, pathophysiology, treatment and prevention of uncomplicated and severe malaria from the three major species causing malaria deaths in our region: Plasmodium falciparum, P. vivax and P knowlesi.
Nick is the recipient of the inaugural Gustav Nossal Medal in Global Health from the Australian Academy of Science and an Honorary International Fellow of the American Society of Tropical Medicine and Hygiene.
Through ongoing collaborations with national and international networks he aims to continue to link basic, clinical and field research to develop new preventative and treatment strategies for malaria.
Research Themes
- The Tropical Disease Regional Research Regional Collaborative Initiative: Responding to Drug-Resistant Tuberculosis and Malaria in the Asia-Pacific
- Comparative pathophysiology of uncomplicated and severe falciparum, vivax and knowlesi malaria
- Immunity and pathogenesis in tropical infectious diseases
- Improving prevention and treatment of uncomplicated and severe falciparum, vivax and knowlesi malaria
- Adjunctive treatment studies targeting endothelial dysfunction and the arginine-nitric oxide pathway in severe falciparum malaria
- Epidemiology and clinical spectrum of vivax and knowlesi malaria
- Tuberculosis pathophysiology and treatment studies.
Pathogenesis
- Kho S, Qotrunnada L, Leonardo L, Andries B, […], Buffet P, Anstey N.M. (2021). Hidden Biomass of Intact Malaria Parasites in the Human Spleen. New England J Medicine; 384(21):2067-2069. doi:10.1056/NEJMc2023884.
- Kho S, Qotrunnada L, Leonardo L, Andries B, […], Buffet P, Anstey N.M. (2021). Evaluation of splenic accumulation and colocalization of immature reticulocytes and Plasmodium vivax in asymptomatic malaria: A prospective human splenectomy study. PLoS Medicine; 18(5):e1003632. doi: 10.1371/journal.pmed.1003632.
- Barber BE, Grigg M, Piera K, Chen Y, William T, Weinberg J, Yeo T, Anstey NM. (2021). Endothelial glycocalyx degradation and disease severity in Plasmodium vivax and Plasmodium knowlesi malaria. Sci Rep;11(1):9741. doi: 10.1038/s41598-021-88962-6.
- Woodford J, Gillman A, Jenvey P, Roberts J, […], Anstey NM, McCarthy JS (2021). Positron emission tomography and magnetic resonance imaging in experimental human malaria to identify organ-specific changes in morphology and glucose metabolism: A prospective cohort study. PLoS Medicine; 18(5):e1003567. doi:10.1371/journal.pmed.1003567.
- Yeo, T.W., Weinberg, J.B., Lampah, D.A., Kenangalem, E., Bush, P., [...], Anstey, N.M. (2019). Glycocalyx Breakdown is Associated with Severe Disease and Fatal Outcome in Plasmodium falciparum Malaria. Clinical Infectious Diseases, 69(10): 1712–1720. doi:10.1093/cid/ciz038.
- Barber, B.E., Grigg, M.J., Piera, K., Amante, F.H., William, T., [...], Anstey, N.M. (2019). Anti-phosphatidylserine IgM and IgG antibodies are higher in vivax than falciparum malaria, and associated with early anemia in both species. The Journal of Infectious Diseases, 220(9):1435–1443. doi:10.1093/infdis/jiz334.
- Kho, S., Barber, B.E., Johar, E., Andries, B., Poespoprodjo, J.R., [...], Anstey, N.M*., McMorran, B*. [*equal contribution] (2018). Platelets kill circulating parasites of all major Plasmodium species in human malaria. Blood, 132(12):1332-1344. doi:10.1182/blood-2018-05-849307.
- Barber, B.E., Grigg, M.J., Piera, K.A., William, T., Cooper, D.J., [...], Anstey, N.M. (2018). Intravascular haemolysis in severe Plasmodium knowlesi malaria: association with endothelial activation, microvascular dysfunction, and acute kidney injury. Emerging Microbes Infection, 7(1):106. doi: 10.1038/s41426-018-0105-2.
- Barber, B.E., Russell, B., Grigg, M.J., Zhang, R., [...], Anstey, N.M*., Yeo, T.W*. [*equal contribution] (2018). Reduced red blood cell deformability in Plasmodium knowlesi malaria. Blood Advances, 2(4): 433-443.
Epidemiology, Surveillance and Strengthening Health Systems
- Currie BJ, Mayo M, Ward LM, Kaestli M, Meumann EM, […], Anstey, N.M. (2021). The Darwin Prospective Melioidosis Study: a 30-year prospective, observational investigation. Lancet Infectious Diseases, S1473-3099(21)00022-0. doi: 10.1016/S1473-3099(21)00022-0.
- Cooper, D.J., Rajahram, G.S., William, T., Jelip, J., Mohammad, R., [...], Anstey, N.M., Barber, B.E. (2020). Plasmodium knowlesi malaria in Sabah, Malaysia, 2015-2017: ongoing increase in incidence despite near-elimination of the human-only Plasmodium species. Clinical Infectious Diseases, 70(3): 361–367. doi:10.1093/cid/ciz237
- Kenangalem, E., Poespoprodjo, J.R., Douglas, N.M., Burdam, F.H., Gdeumana, K., [...], Anstey N.M., Price, R.N. (2019). Malaria morbidity and mortality following introduction of a universal policy of artemisinin-based treatment for malaria in Papua, Indonesia: a longitudinal surveillance study. PLoS Medicine 16(5): e1002815. doi: 10.1371/journal.pmed.1002815.
- Grigg, M.J., Cox, J., William, T., Jelip, J., Fornace, K.M., [...], Anstey, N.M., Yeo, T.W., Drakeley, C.J. (2017). Individual factors associated with the risk of acquiring human Plasmodium knowlesi malaria in Malaysia: a case-control study. Lancet Planet Health, 1(3), e97–e104. doi: 10.1016/S2542-5196(17)30031-1.
- Grigg, M.J., William, T., Piera, K.A., Rajahram, G.S., Jelip, J., [...], Anstey, N.M. (2017). Plasmodium falciparum artemisinin resistance monitoring in Sabah, Malaysia: in vivo therapeutic efficacy and kelch13 molecular marker surveillance. Malaria Journal, 17(1):463. doi: 10.1186/s12936-018-2593-x.
Clinical trials, meta-analyses and systematic reviews
- Mousa A, Al-Taiar A, Anstey NM, […], Okell LC (2020). The impact of delayed treatment of uncomplicated P. falciparum malaria on progression to severe malaria: A systematic review and a pooled multicentre individual-patient meta-analysis. PLoS Medicine - doi.org/10.1371/journal.pmed.1003359
- Rajahram, G.S., Cooper, D.J., William, T., Grigg, M.J., Anstey, N.M. and Barber, B.E. (2019). Deaths from Plasmodium knowlesi malaria: case series and systematic review. Clinical Infectious Diseases. 69(10):1703–1711. doi:10.1093/cid/ciz011.
- Commons, R.J., Simpson, J.A., Thriemer, K., Abreha, T., Adam, I., Anstey, N.M., [...], Price, R.N. (2019). The efficacy of dihydroartemisinin-piperaquine and artemether-lumefantrine with and without primaquine on Plasmodium vivax recurrence: a systematic review and individual patient data meta-analysis. PLoS Medicine, 16(10): e1002928. doi: 10.1371/journal.pmed.1002928.
- Grigg, M.J., William, T., Barber, B.E., Rajahram, G.S., Menon, J., [...], Anstey, N.M. (2018). Artemether-lumefantrine versus chloroquine for the treatment of uncomplicated Plasmodium knowlesi malaria: an open-label randomized controlled trial (CAN KNOW). Clinical Infectious Diseases, 66(2): 229-236. doi: 10.1093/cid/cix779.
- Commons RJ, Simpson JA, Thriemer K, Humphreys GS, Abreha T, Alemu SG, Añez A, Anstey NM, […], Price, R.N. (2018). The effect of chloroquine dose and primaquine on Plasmodium vivax recurrence: a WorldWide Antimalarial Resistance Network systematic review and individual patient pooled meta-analysis. Lancet Infectious Diseases, 18(9): 1025-1034. doi: 10.1016/S1473-3099(18)30348-7.
- Douglas, N.M., Poespoprodjo, J.R., Patriani, D., Malloy, M.J., Kenangalem, E., [...], Anstey N.M., Price, R.N. (2017). Unsupervised primaquine for the treatment of Plasmodium vivax malaria relapses in southern Papua: a hospital-based cohort study. PLoS Medicine, 14(8): e1002379. doi: 10.1371/journal.pmed.1002379.
Clinical spectrum
- Anstey, N.M., Grigg, M.J., Rajahram, G.S., […], Kho, S, Barber, B.E (2021). Knowlesi malaria: human risk factors, clinical spectrum, and pathophysiology. Advances Parasitology, 113 in press
- Kho, S., Andries, B., Poespoprodjo, J.R., Commons, R.J., Shanti, P.A.I., [...], Anstey, N.M., Price, R.N. (2019). High risk of Plasmodium vivax malaria following splenectomy in Papua, Indonesia. Clinical Infectious Diseases, 68(1):51-60. doi: 10.1093/cid/ciy403.
- Grigg, M.J., William, T., Barber, B.E., Rajahram, G.S., Menon, J., [...], Anstey, N.M. (2018). Age-related clinical spectrum of Plasmodium knowlesi malaria and predictors of severity. Clinical Infectious Diseases 67(3):350-359. doi: 10.1093/cid/ciy065.
- Aung, N.M., Nyein, P.P., Htut, T.Y., Htet, Z.W., Kyi, T.T., Anstey, N.M., [...], Hanson, J. (2018). Antibiotic Therapy in Adults with Malaria: High Rate of Clinically Significant Bacteremia in Hospitalized Adults Diagnosed with Falciparum Malaria. The American Journal of Tropical Medicine and Hygiene, 99(3): 688–696. doi:10.4269/ajtmh.18-0378.
Click here to view more Nick Anstey publications in PubMed.
-
MEDIA RELEASE | Menzies researchers RESPOND to priority diseases in our global neighbourhood
Menzies will lead a 4-year health system strengthening partnership in the Asia-Pacific region, under the Partnerships for a Healthy Region Initiative by the Australian Government.
-
MEDIA RELEASE | Menzies researchers in the top 2 per cent
Menzies School of Health Research is celebrating the work of its researchers who have been ranked amongst the world’s top scientists.
-
Medical Express | Using paracetamol for protecting kidneys in patients with severe malaria
Dr. Daniel Cooper said the findings are important because they will help provide the best possible treatment to patients with severe malaria.
-
Using paracetamol for protecting kidneys in patients with severe malaria
Paracetamol is used in many illnesses for the relief of pain and fever, but a study just published in Clinical Infectious Diseases has shown that it may also help protect against kidney damage in patients with malaria.
-

Researchers at CDU some of the most influential in their fields
According to a Stanford University study, there were 22 academics from CDU and Menzies School of Health research who ranked in the top two per cent of researchers referenced in their respected disciplines for 2020.
-
.jpg&w=123&h=126)
Parasit malaria bersembunyi di organ limpa
-

Parasit Malaria Bisa Bersembunyi di Limpa Manusia
Studi terbaru mengungkapkan, parasit malaria terbukti lebih banyak yang bersembunyi dan berkembang biak di dalam limpa manusia. Temuan tersebut mendefinisikan ulang siklus hidup malaria.
-

Penelitian Berhasil Ungkap Parasit Malaria Bersembunyi di Limpa Sumber: https://mediaindonesia.com/humaniora/408850/penelitian-berhasil-ungkap-parasit-malaria-bersembunyi-di-limpa
LEMBAGA Biologi Molekuler Eijkman mengatakan hasil penelitian yang dilakukan Eijkman dan rekannya menunjukkan sejumlah besar parasit malaria ternyata bersembunyi di organ limpa.
-
.jpg&w=123&h=126)
Parasites may accumulate in spleens of asymptomatic individuals infected with malaria
Study suggests immature red blood cells in spleen are targeted for invasion by P. vivax.
-

Malaria is not only a blood disease, it also hides in the spleen, scientists have discovered
Groundbreaking new research has found large numbers of malaria parasites hiding in the spleen. Until now, it was thought that once malaria parasites reached the bloodstream, they circulated and multiplied only in the blood.
-
Hidden malaria life cycle discovered in the spleen
Ground-breaking studies published today in the New England Journal of Medicine and PLOS Medicine have found large numbers of malaria parasites hiding in the human spleen where they actively multiply in a previously unrecognised life cycle.
-

CDU academics named among world’s most influential
Menzies School of Health Research Professor Bart Currie, Professor Anne Chang AM, Professor Ric Price, Associate Professor Steven Tong, Professor Nicholas Anstey, Professor Joshua Davis, Professor Alan Cass, Professor Peter Morris and Professor Amanda Leach
-
An open letter from 119 scientists and researchers to The Lancet
Signed by clinicians, medical researchers, statisticians, and ethicists from across the world, follows the publication of a paper on using hydroxychloroquine or chloroquine for the treatment of COVID-19.
-
How we can end TB by 2030
A regional research collaboration with the Menzies School of Health Research has been highly productive in building capacity in PNG and Indonesia,.
-
CDU, Menzies researcher leads battle against malaria
National Tribune Online news | Graduating this week with a PhD, rising star malaria researcher Dr Steven Kho.
-
MediaNewsroomCDU, Menzies researcher leads battle against malaria CDU, Menzies researcher leads battle against malaria
Blood platelets, neutrophils and the spleen have novel roles in people with malaria, according to new research from Charles Darwin University (CDU) and Menzies School of Health Research.
-
Asia–Pacific research partnerships set to tackle big challenges
The largest grant, of $257,767, goes to the Menzies School of Health Research for a project with collaborators in Bangladesh, Indonesia and the Netherlands.
-
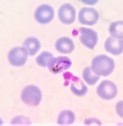
Research reveals defence against malaria parasites
The study, which has just been published in the prestigious journal Blood, was led by Associate Professor Brendan McMorran at ANU and Professor Nick Anstey at Darwin's Menzies School of Health Research
-
Xinhuanet.com|Platelets kill up to 60 pct of malaria parasites: Australian study
The study, published by the Menzies School of Health Research (MSHR) in Australia's Northern Territory (NT), revealed that platelets attack and kill malaria parasites in the bloodstream.
-
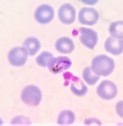
Platelets the first line of defence in malaria patients
The humble platelet is usually regarded as just a tiny cell that helps the blood clot. A study just published in the prestigious journal Blood has found that platelets attack and kill malaria parasites in infected humans to reduce the number of parasites circulating in their blood.
-
New evidence supports radical treatment of widespread form of malaria
A team of malaria experts from a large international research collaboration has today published results supporting the need for a radical cure strategy to tackle one of the most debilitating forms of malaria caused by the Plasmodium vivax parasite.
-

Award no tall order for Matthew - Darwin Sun
A DARWIN scientist has been named the Young Tall Poppy Scientist of the Year in recognition of his research into a type of monkey malaria transmitted to humans via mosquitoes.
-
NT News | Brains Trust Born
Researchers at Darwin's Menzies School of Health Research will play a key role in a new push to fight the scourge of malaria in the Asia-Pacific region.
-
Monkey malaria researcher named NT Young Tall Poppy
Menzies School of Health Research (Menzies) clinical research fellow Dr Matthew Grigg has been named the 2017 NT Young Tall Poppy Scientist of the Year in recognition for ongoing research into Plasmodium knowlesi (P. knowlesi) malaria, a type of monkey malaria transmitted to humans via mosquitos in Southeast Asia.
-
New Australian-led malaria research powerhouse gears up to hunt down malaria across the Asia-Pacific
Australia will take a leadership role in the Asia-Pacific region in a new initiative to help our nearest neighbours rid the scourge of malaria, in a new National Health and Medical Research Council (NHMRC) Centre for Research Excellence in Malaria Elimination.
-

Territory Q features HOT NORTH
Read about our HOT NORTH collaboration in the latest Territory Q Magazine.
-
Adult male farmers most at risk of contracting monkey malaria in Malaysia
Lead author, Menzies School of Health Research research fellow, Dr Matthew Grigg has specialised in identifying and researching risk factors and treatment for P. knowlesi malaria in Sabah, Malaysian Borneo.
-

$2m grant to combat drug resistant malaria and tuberculosis
A $2m research grant to work towards the prevention, control and elimination of malaria and tuberculosis (TB) in Southeast Asia and the Pacific has been awarded to a consortium led by Menzies School of Health Research, in collaboration with Burnet Institute, the Department of Foreign Affairs and Trade announced today.
-

TerritoryQ: War on Malaria, Prof Ric Price and Prof Nicholas Anstey
A medical team based in Darwin has put itself at the centre of the goal to eliminate malaria from the Asia-Pacific
-

Menzies leaders inducted into important new health and medical academy
Three Menzies researchers inducted as Fellows of the newly formed Australian Academy of Health and Medical Sciences.
-

Infectious diseases specialist honoured with prestigious Academy Award
One of Australia’s leading infectious diseases specialists has been recognised with a prestigious national award for his contributions in tackling the global burden of malaria.
-

Menzies secures critical funding for malaria and tropical health research
The millions of people worldwide who suffer from malaria and other tropical infections each year will benefit from the awarding of a federal fellowship to one of the country's leading clinical researchers in tropical health.













