Project team:
Chief investigator:
- Professor Richard Price
Project manager:
-
Contact Catherine Martel for further information about the study.
Investigators:
- Dr. Kamala Ley-Thriemer - Menzies School of Health Research, Darwin, Australia
- Dr. Benedikt Ley - Menzies School of Health Research, Darwin, Australia
- Dr. Lorenz von Seidlein - Mahidol-Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
- Dr. Bob Taylor - Mahidol - Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
- Professor Nicholas Day - Mahidol-Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
- Professor Arjen Dondorp - Mahidol-Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
- Dr. Mehul Dhodra Mahidol - Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
- Dr. Phaik Yeong Cheah - Mahidol-Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
- Prayoon Yuentrakul - Mahidol-Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
- Professor Nicholas White - Mahidol-Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
- Dr. Awab Ghulam Rahim - Malaria Control Centre, Jalalabad, Afghanistan
- Dr. Yoel Lubell - Mahidol-Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
- Dr. Kevin Baird - Eijkman Oxford Clinical Research Unit (EOCRU), Jakarta, Indonesia
- Dr. Ayodhia Pasaribu - Department of Paediatrics, Medical Faculty, University of Sumatera Utara, Indonesia
- Professor Inge Sutanto - University of Indonesia, Jakarta, Indonesia
- Professor Tran Tinh Hien - Oxford University Clinical Research Unit (OCRU), Ho Chi Minh City, Vietnam
- Professor Asrat Hailu Mekuria - Addis Ababa University, School of Medicine, Addis Ababa, Ethiopia
- Dr. Tamiru Degaga – Arba Minch University, Ethiopia
- Dr. Adugna Woyessa - Ethiopia Public Health Institute (EPHI), Addis Ababa, Ethiopia
- Dr. Ashenafi Assefa - Ethiopia Public Health Institute (EPHI), Addis Ababa, Ethiopia.
Funders:
This research was funded by the:
- UK Department for International Development, UK Medical Research Council, UK National Institute for Health Research, and the Wellcome Trust through the Joint Global Health Trials Scheme (MR/K007424/1)
- Bill & Melinda Gates Foundation (OPP1054404).
Collaborators:
- Mahidol-Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
- Malaria Control Centre, Jalalabad, Afghanistan
- Eijkman Oxford Clinical Research Unit (EOCRU), Jakarta, Indonesia
- University of Indonesia, Jakarta, Indonesia
- Department of Paediatrics, Medical Faculty, University of Sumatera Utara, Indonesia
- Oxford University Clinical Research Unit (OUCRU), Ho Chi Minh City, Vietnam
- Addis Ababa University, School of Medicine, Addis Ababa, Ethiopia
- Arba Minch University
- Ethiopia Public Health Institute (EPHI), Addis Ababa, Ethiopia.
Photo credits:
- Pearl Gan in association with OUCRU, Vietnam and EOCRU, Indonesia.
A multicentre randomised, placebo-controlled comparison of short and long course primaquine regimens (IMPROV)
Aim:
This clinical trial assessed the efficacy and safety of a short-course high dose primaquine regimen for the radical cure of vivax malaria.
Rationale:
Outside of sub-Saharan Africa, malaria is caused by two main parasites: Plasmodium falciparum and Plasmodium vivax. P. vivax forms dormant liver stages that reactivate weeks or months following an acute infection and can lead to severe or life-threatening disease. The WHO currently recommends a treatment with 14 days of primaquine to kill the liver stage parasites, but the long course of treatment means that many patients don’t complete their medication and fail treatment.
This large clinical trial enrolled 2388 patients at eight sites and treated them with high dose primaquine (total dose 7mg/kg) administered either over 14-days (0.5mg/kg/day) or 7 days (1mg/kg/day). Patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency, an inherited disorder found in up to 20% of some populations, are at risk of drug-induced haemolysis which causes severe anaemia. All patients were tested for G6PD before being treated.
Our research has found:
In G6PD normal patients, the 7-day primaquine regimen was well tolerated and non-inferior to 14-day primaquine. In all sites, both primaquine regimens had almost 90% cure rates compared to a relapse rate of 50% in patients not treated with primaquine.
Implications for policy and practice:
The findings have important implications for the treatment and elimination of vivax malaria in the Asia-Pacific, the Horn of Africa and the Americas. The short-course regimen has potential to improve adherence and therefore effectiveness of primaquine for the radical cure of P. vivax. A policy of testing for G6PD deficiency and treating with short-course high-dose primaquine is now being considered by several malaria endemic countries. Further studies are underway to study the safety and effectiveness of this regimen in clinical practice.
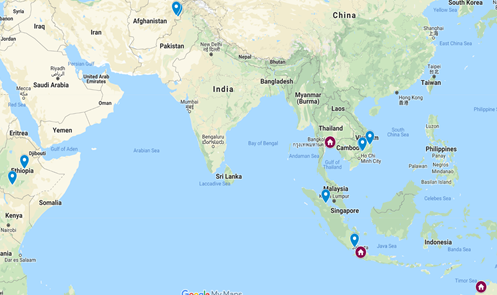
Our research locations:
- Afghanistan
- Indonesia
- Ethiopia
- Vietnam.
- Taylor, W., Thriemer, K. et al. (2019). Short-course primaquine for the radical cure of Plasmodium vivax malaria: a multicentre, randomised, placebo-controlled non-inferiority trial. Lancet, 394(10202), 929–938. doi:10.1016/S0140-6736(19)31285-1 https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(19)31285-1/fulltext
Paper on lessons learnt from dissemination of IMPROV results to trial participants
-
Degaga, T. S., Weston, S., Tego, T. T., Abate, D. T., Aseffa, A., Wayessa, A., Price, R. N., Hailu, A., & Thriemer, K. (2020). Disseminating clinical study results to trial participants in Ethiopia: insights and lessons learned. Malaria Journal, 19, 1-6. [205]. https://doi.org/10.1186/s12936-020-03279-5
Paper on the ethical considerations of using placebo control arms in a radical cure clinical trial
- Cheah, P. Y., Steinkamp, N., von Seidlein, L., & Price, R. N. (2018). The ethics of using placebo in randomised controlled trials: a case study of a Plasmodium vivax antirelapse trial. BMC Medical Ethics, 19(1), 19. doi:10.1186/s12910-018-0259-4 https://www.ncbi.nlm.nih.gov/pubmed/29510711
Published IMPROV Study protocol
- IMPROV Study Group. (2015). Improving the radical cure of vivax malaria (IMPROV): a study protocol for a multi-centre randomised, placebo-controlled comparison of short and long course primaquine regimens. BMC Infectious Diseases,15,558. doi: 10.1186/s12879-015-1276-2 https://www.ncbi.nlm.nih.gov/pubmed/26643116
Publication of the patient and societal costs of P. vivax derived from the IMPROV clinical trial
- Devine, A., Pasaribu, A. et al. (2010). Provider and household costs of Plasmodium vivax malaria episodes: a multicountry comparative analysis of primary trial data. (2019). Bulletin of the World Health Organisation, 97. doi:http://dx.doi.org/10.2471/BLT.18.226688 http://www9.who.int/bulletin/online_first/en/
Other resources:
Results have been presented at the following conferences:
- ASTMH 67th Annual Meeting, Session 167, Symposium “Short Course Primaquine Regimen for the Radical Cure of Plasmodium vivax” New Orleans, October 28 - November 1, 2018
- 7th International Conference on Plasmodium vivax Research (ICPvR), Paris, June 26-28, 2019
- The Malaria Endgame: Innovation in Therapeutics, Vector Control and Public Health Tools (G1), Keystone Symposia on Molecular and Cellular Biology, Addis Ababa, Ethiopia, October 30—November 2, 2019
Engagement with Policy Makers and National Malaria Programs
- APMEN: The results of the IMPROV study were presented at the Vivax Working Group meeting in Kathmandu, Nepal on 15-17th October 2019.
- Indonesia: The results of the IMPROV study were presented and reviewed at the Indonesian National Malaria Expert Committee, the 24th October 2019.
- Ethiopia: The results of the IMPROV study were presented and reviewed at a stakeholder meeting including representatives from the NMCP, the Technical Advisory Group, WHO, Malaria Consortium, PATH, Addis Continental Institute of Public Health, and the Ethiopian Public Health Institute, the 8th November 2019.
Public Engagement:
To feedback results of the trial to patients enrolled in the study, easy to understand flyers were designed. Flyers were translated into local language of all participating sites.
In addition, community consultations are currently done and/ or planned to feedback results to patients. Patient feedback from the study site in Arba Minch, Ethiopia included comments such as:
“Before the study I was suffering 10 times per year from malaria, since the study I had no more malaria” (young female patient).
“This research shows we need primaquine and it should be made available” (male patient approx 40 years old).
“We need more research also in other diseases like typhoid” (male patient, approx. 30 years old).

Community consultation, November 2019, Arba Minch, Ethiopia.
Study title:
A multicentre randomised, placebo-controlled comparison of short and long course primaquine regimens (IMPROV).
Study purpose:
- To assess the efficacy of a shorter course (7 days) of primaquine for radical cure of vivax malaria.
Objectives:
Primary
- To determine whether a 7-day primaquine regimen is safe and not inferior to the standard 14-day regimen (total dose of 7mg/kg in both arms) in preventing P. vivax relapse in G6PD normal patients.
Secondary
- To assess the absolute risks and benefits of radical treatment regimens in different endemic settings. To provide data on the safety of a weekly dose of primaquine (0.75 mg base/kg) in patients with G6PD deficiency.
- To identify the most cost-effective strategies for the management of P. vivax with respect to the use of G6PD tests, the dosing schedule and the epidemiological context
For more information visit the clinical trials website.
Project dates:
The project commenced in July 2014 and concluded in November 2017.