Click here for information on the Engaging Stakeholders in Identifying Priority Evidence-Practice Gaps and Strategies for Improvement (the ESP Project).
From 2010 to 2015 the ABCD National Research Partnership (The Partnership) worked across states and territories in Australia to improve the quality of primary health care available to Indigenous people. Using participatory action research approaches, The Partnership aimed to:
- investigate the variation in quality of care in Indigenous primary health care (PHC) centres
- explore the underlying factors associated with variation at the health centre and regional level
- identify and examine specific strategies that have been effective in improving primary care clinical performance
- work with health service staff, management and policy makers to enhance the effective implementation of successful strategies.
Click here to download a printable version of the project information sheet.
Background:
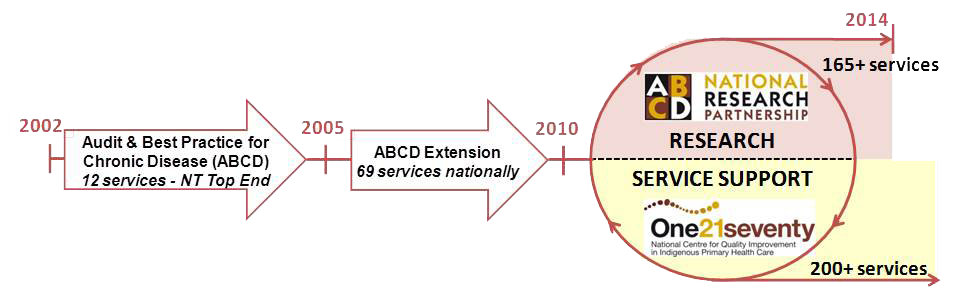
The ABCD project originated in 2002 in the Northern Territory with the ABCDE project continuing this work from 2005-2009. By the end of 2009 over 140 health centres around Australia were using ABCD tools and processes to improve their quality of care.
The projects provided support for the development and use of audit tools and processes and a web-based database and reporting system for Primary Health Care centres around Australia. Following requests from users for continued use of the tools and processes, One21Seventy, the National Centre for Quality Improvement in Indigenous Health was established in November 2009. This organisation, based in Menzies, provided tools and processes, including training, to support primary health care providers to carry out Continuous Quality Improvement (CQI) using clinical audits, systems assessment, web-based data analysis and reporting to inform goal setting and action planning.
The Partnership worked alongside One21Seventy to continue to develop the evidence-base available to One21Seventy and to answer key questions relevant to quality improvement in the sector. The Partnership accessed data collected in routine CQI activities from services that had consented to participate with the Partnership for research.
Timeline progression of the ABCD Partnership Project:
Our funders, supporters and partners:
The ABCD National Research Partnership Project was supported by funding from the National Health and Medical Research Council and the Lowitja Institute, and by in-kind and financial support from a range of Aboriginal Community Controlled organisations and Government agencies. The Lowitja Institute provided support to employ research officers in two jurisdictions and to support the development of audit tools and processes. beyondblue has provided funding for the development and implementation of the Youth Health tool.
Our partners:
The ABCD NRP worked in partnership with partners from Aboriginal Community Controlled Health Organisation peak bodies, government health departments, academic institutions, and Primary Health Care (PHC) services in five states and territories: the Northern Territory, Queensland, South Australia, Western Australia and New South Wales. Many of the partners participated in the ABCD project and have maintained their engagement in improving the quality of care through the Partnership project.
National and regional research program:
The Partnership aimed to:
- investigate the variation in quality of care in Indigenous primary health care (PHC) centre
- explore the underlying factors associated with variation at the health centre and regional level
- identify and examine specific strategies that have been effective in improving primary care clinical performance.
Click here to download a Research Focus 2010-2014 brochure.
The research program utilised expertise and skills from academia, policy and service levels across Australia and is focussed on the project objectives. The Partnership provided a structure that facilitated service and policy driven research that was cross jurisdictional, cross sector and trans-disciplinary. This collaborative approach and access to a national data set provided opportunities for analysis at a national level and for more in-depth research to achieve the objectives of the project.
National research priorities were identified through analysis of the national data set, consideration of emerging health issues, and areas of common interest across jurisdictions. Regional research priorities were identified by state and territory steering committees supported by State and Territory Research Officers who facilitated this process through consultation with service providers and policy makers.
A collaborative approach that included active involvement of end users throughout the process, from identification of research topics to implementation, was used to develop and implement research projects to address identified priorities. Each project had an advisory/reference group comprising end users, key stakeholders and experts, including service providers, clinical experts, policy makers and quality improvement experts.
Data were extracted from the One21seventy web-based database for services who agreed to participate in the Partnership. Individual client data and service names were de-identified and any identifying information was not published without the prior consent of the service. Data at the national and jurisdictional level were available to researchers for projects that were approved by the Research sub-committee and had ethics approval.
Research under the Partnership had to have ethics clearance from the relevant ethics committee and have approval from the Partnership Research Subcommittee. This committee consisted of seven members including academics and health department researchers from NT, WA, Qld and the PCC, and oversaw all aspects of the research program, strengthening research projects through feedback to researchers. This included providing advice and support on the development and implementation of projects, assessing and approving projects, monitoring progress and advice and approval of manuscripts for publication, policy briefs, or research reports. Researchers were required to submit an Expression of Interest to the Research Subcommittee prior to accessing data.
Click on the following poster links for further details of the national and regional research program:
- CQI + Research + Change Advocates = Improvements in Primary Health Care
- How PHC services can improve quality of care through CQI research and shared learning.
Participating Primary Health Care (PHC) Centres:
As at July 2013, 165 PHC centres (132 Government health services and 33 community controlled services) had agreed to participate in the research project. This was formalised by signing the ABCD National Research Partnership Agreement between Menzies, the PHC centre or Health Department and the Regional Project Leader. The PHC centres agreed to contribute their de-identified CQI data from the One21seventy data base into a national pool for broad analysis of variation in health care delivery and to answer key questions of relevance to policy and practice. They also had an option to participate in more in-depth studies and to lead and/or participate in research driven by locally identified needs.
This map gives an overview of the location of the health services that were involved in the Partnership:

Routine analysis of variation in care:
- Analysis of national and jurisdictional data, Menzies School of Health Research
- Extent of screening for post natal depression in Aboriginal and Torres Strait Island women, Combined Universities Centre for Rural Health (CUCRH)
- Longitudinal analysis of maternal health data, Monash University.
Factors underlying variation / Contextual analysis:
- Childhood anaemia, Menzies School of Health Research
- Competing demands in primary care – the case of depression in diabetes, Menzies School of Health Research
- What are the characteristics of health services who demonstrate improvement in quality of care? CUCHR, James Cook University
- Realist Analysis - effectiveness of CQI in complex primary health care environments, Menzies School of Health Research
- Community environmental conditions and risk factors for cardio metabolic disease, University of South Australia.
Analysis of what kinds of interventions work:
- Investigating the barriers and enablers to Continuous Quality Improvement (CQI) within Aboriginal primary health care services in South Australia, Aboriginal Health Council of South Australia
- Qualitative strengths-based evaluation of Indigenous health centre participation in CQI in Australia, International student Menzies. CQI success stories summary
- Supporting CQI within Indigenous PHC – identifying and exploring effective strategies, University of South Australia.
Other issues:
- ABCD NRP: development of conceptual model incorporating practice-based research networks, system-based PAR and CQI in community-based PHC (incorporates literature review of all elements), Menzies School of Health Research
- TRAK - Talking about Raising Aboriginal Kids - an evaluation of an early childhood education intervention for remote Aboriginal Health Workers, Menzies School of Health Research.
Information brochures:
- ABCD National Research Partnership – Research Focus 2010-2014 brochure
- ABCD National Research Partnership – Improving Practice through Research brochure
- Data Dictionary
- Information for researchers - National Research Partnership to improve primary health care performance and outcomes for Indigenous peoples flyer.
Publications:
- Matthews, V., Schierhout, G., McBroom, J., Connors, C., Kennedy, C., Kwedza, R., Larkins, S., Moore, E., Thompson, S., Scrimgeour, D., & Bailie R. (2014). Duration of CQI participation: a key factor explaining improvement in delivery of Type 2 diabetes services to Aboriginal and Torres Strait Islander communities. BMC Health Services Research,14, 578.
- O’Donoghue, L., Percival, N., Laycock, A., McCalman, J., Tsey, K., Armit, C., & Bailie, R. (2014). Evaluating Aboriginal and Torres Strait Islander health promotion activities using audit and feedback. Australian Journal of Primary Health, 20, 339-344.
- Bailie, R., Matthews, V., Brands, J., & Schierhout, G.(2013). A systems-based partnership learning model for strengthening primary health care. Implementation Science, 8,143.
- Ralph, A., Fittock, M., Schultz, R., Thompson, D., Dowden, M., Clemens, T., Parnaby, M., Clark, M., McDonald, E., Edwards, K., Carapetis, J., & Bailie, R. (2013). Improvement in rheumatic fever and rheumatic heart disease management and prevention using a health centre-based continuous quality improvement approach. BMC Health Services Research, 13, 25.
- Schierhout, G., Hains, J., Si, D., Kennedy, C., Cox, R., Kwedza, R., O’Donoghue, L., Fittock, M., Brands, J., Lonergan, K., Dowden, M., & Bailie, R. (2013). Evaluating the effectiveness of a multifaceted, multilevel continuous quality improvement program in primary health care: developing a realist theory of change. Implementation Science, 8,119.
- Schierhout, G., Nagel, T., Si, D., Connors, C., Brown, A., & Bailie, R. (2013). Do competing demands of physical illness in Type 2 diabetes influence depression screening, documentation and management in primary care: a cross-sectional analytic study in Aboriginal and Torres Strait Islander primary health care settings. International Journal of Mental Health Systems, 7,16.
- Si, D., Dowden, M., Kennedy, C., Cox, R., O’Donoghue, L., Liddle, H., Kwedza, R., Connors, C., Thompson, S., Burke, H., Brown, A., Weeramanthri, T., Schierhout, G., & Bailie, R. (2011). Indigenous community care: Documented depression in patients with diabetes. Australian Family Physician, 40(5),331-333.
- Bailie, R., Si, D., Connors, C., Kwedza, R., O'Donoghue, L., Kennedy, C., et al. (2011). Variation in quality of preventive care for well adults in Indigenous community health centres in Australia. BMC Health Services Research, 11(1) 139.
- Rumbold, A., Bailie, R., Si, D., Dowden, M., Kennedy, C., Cox, R., et al. (2011). Delivery of maternal health care in Indigenous primary care services: baseline data for an ongoing quality improvement initiative. Pregnancy and Childbirth, 11(1),16.
- Bailie, R., Si, D., Shannon, C., Semmens, J., Rowley, K., Scrimgeour, D.J., et al. (2010). Study protocol: national research partnership to improve primary health care performance and outcomes for Indigenous peoples. BMC Health Services Research,10,129.