The Engaging Stakeholders in Identifying Priority Evidence-Practice Gaps and Strategies for Improvement (ESP) Project. (2014 - 2017)
Project aims:
The aims of the ESP Project were to:
- Distribute reports of aggregated continuous quality improvement (CQI) data from Aboriginal and Torres Strait Islander health centres and services
- Engage a wide range of stakeholders in using the data to identify and address system-wide 'evidence-practice gaps' in Aboriginal and Torres Strait Islander primary health care (PHC)*
*An 'evidence-practice' gap is an important item of recommended health or clinical care that is provided to fewer people than expected.
Background:
The CQI data used in the ESP project were collected over ten years from 175 health centres and services using the One21seventy tools and processes and participating in the ABCD National Research Partnership. Approximately 60,000 de-identified clinical audits of patient records and 492 systems assessments related to six areas of care:
- child health
- chronic illness (vascular and metabolic)
- rheumatic heart disease
- mental health and wellbeing
- preventive health
- maternal health.
Project description:
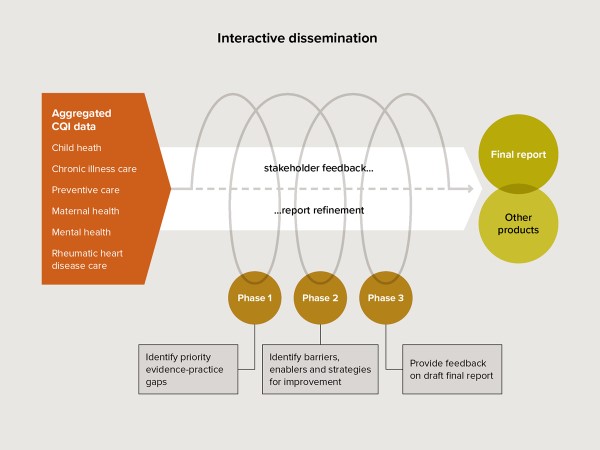
ESP reports of aggregated data were emailed through the existing ABCD National Research Partnership network and a snowballing recruitment technique was used to invite wider participation. People in different roles and across different levels of the PHC system provided feedback through online surveys. A phased reporting and feedback process was used, culminating in a final report and other products in each area of care (Figure 1).
Phase 1:
Identification of priority evidence-practice gaps.
A preliminary analysis report of aggregated cross-sectional CQI data was distributed with a linked survey.
Phase 2:
Identification of barriers, enablers and strategies for addressing identified gaps in care.
A report of trend data relevant to the identified priority evidence-practice gaps was distributed with a survey about influences on individual behaviours, the health centre and wider systems and strategies stakeholders would suggest for modifying barriers and strengthening enablers.
Phase 3:
Provision of feedback on draft final report:
The report was distributed with a survey gathering feedback on the draft overall findings.
A concurrent development evaluation guided the team in refining the ESP design, reports and processes. The evaluation also explored facilitators and barriers to stakeholder engagement with the data, how stakeholders used the ESP project findings and how well the interactive dissemination processes worked overall.
Outputs:
Research outputs included six technical reports, ten summaries of findings and/or key messages, eight publications in peer-reviewed journals, presentations and posters at 18 national and international conferences, and three parliamentary submissions.
Extensive input from stakeholders (over 900 people) across the different areas of care meant the project provided a capacity building element in the use of aggregated CQI data. Further research projects have been developed based on needs identified though the ESP project.
Key findings:
The project identified a set of priority gaps in care, barriers to addressing these and strategies for each area of care. Evidence practice-gaps across areas of care included:
- Follow-up of abnormal clinical findings and laboratory results
- The recording of risk factors and of brief interventions
- Emotional wellbeing assessment and support
- Systems to strengthen links between communities and health services.
Commonly identified barriers to improvement included:
- Workforce recruitment and retention issues
- The training and development of health staff
- The development and effective use of clinical information systems
- Systems to support patient-centred care
- Effective use of data to inform decision making
- Management training and support for CQI
- Links between communities and health services.